News Story
BioE Capstone 2015: New Projects Focus on Sensorineural Hearing Loss, Injury Rehabilitation, and More

Members of the BioE Class of 2015 with their mentors, BioE faculty and Capstone judges.
Demonstrating firsthand bioengineering’s enormous potential to change lives through human health innovation, the Fischell Department of Bioengineering (BioE) 2015 Senior Capstone class exhibited a total of 18 novel concepts during the Capstone II finale on May 13, 2015.
Projects ranged from a dynamic pressure-relieving medical mattress and a clinical sleeve for ACL injury risk assessment to a portable stroke rehabilitation system and a device to reduce eye pressure in glaucoma patients.
The 2015 Capstone Design Competition marked the biggest yet, as 91 students pitched their products to a panel of esteemed judges, as well as to BioE faculty and fellow students. Created and sponsored by Mrs. Susan Fischell, wife of A. James Clark School benefactor Dr. Robert E. Fischell, the Capstone Design Competition has been a marquee event, capping off the end of the academic year.
This year's panel of judges included:
- Dr. Dean Chang, Associate Vice President of Innovation and Entrepreneurship, Academy for Innovation and Entrepreneurship, University of Maryland
- Ms. Stefanie Cohen and Mr. Shawn Greenspan, members of the 2014 Bioengineering Capstone Design Competition 1st Place group
- Dr. Zeynep Erim, Program Officer, Division of Interdisciplinary Training, National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health
- Mr. Jeffrey Gibbs, Hyman Phelps & McNamara
- Dr. John Karanian, Director of the Cardiovascular Therapeutics Lab at the Food and Drug Administration’s Center for Devices and Radiological Health
- Mr. Brian Lipford, Vice President of Operations, QA Manager, Key Tech
- Ms. Abbie Shoemaker, Senior Electrical Engineer, Key Tech
- Dr. Gayatri Varma, Executive Director, Office of Technology Commercialization, University of Maryland
- Dr. Jafar Vossoughi, President, Biomed Research Foundation, and Adjunct Professor, University of Maryland
- Ms. Kim Wallace, Director of Program Management and Finance, Academy for Innovation and Entrepreneurship, University of Maryland
- Mr. David Wise, The Genetics & IVF Institute
2015 Capstone II Teams, Projects and Awards
Team 1: Reducing Eye Pressure and Deformation in Glaucoma Patients
Margaret Prendergast, Abigail Iacangelo, Henry Ko, Jonathan Kozlowski, and Rebecca Zubajlo
Advisors: Dr. Ian White (Associate Professor, BioE), Dr. Lex Schultheis (Research Professor, BioE, Director, FDA Regulatory Science and Innovation Initiative), and Dr. Alison Flatau (Department of Aerospace Engineering Professor and Associate Dean for Research)

Research has shown that deterioration of ganglion cells in glaucoma patients is exacerbated by extended intraocular pressure (IOP) increases. Recent results also show that deformation of the eye while sleeping in non-supine positions causes strain in the wall of the eye that are of the same magnitude as IOP increases of elevations in pressure of 1-6 mm Hg. Preliminary eye shield designs have been shown to prevent these pressure spikes, but are currently uncomfortable to wear during sleep.
With this in mind, Capstone Team 1 designed and tested the compliance and comfort of new eye shields to be worn by patients with glaucoma while sleeping. The team successfully redesigned existing preliminary eye shields to be comfortable enough to be worn throughout the night during sleep. Eye shields were fabricated from geometric renderings of each participant’s unique facial surface and then manufactured using a fused deposition modeling (FDM) 3-D printing system. The eye shields were designed to shift pressure away from critical facial regions that may affect IOP.
After multiple design iterations, Team 1 settled on two forms of eye shield design and began to evaluate comfort. Both design designations A and B featured two mirror-image pieces of ABS plastic, one over each eye, mounted on a foam lining wrapped around the outside of the eye, from the zygomatic arch to the center of the forehead. Design A was a plastic mounted around the eye; whereas, design B included an additional guard over – without touching – the eye, which directly protected the area from any external contact.
Twenty people of various age, gender and ethnicity participated in this comfort and compliance study. First, each participant had his or her face scanned with an Xbox Kinect 2.0 device. Facial geometries were rendered and exported as STL files to be modified into designs A and B in Meshmixer. Standardized-sized masks were also fabricated using SolidWorks and open-source facial dimension databases. Participants were asked to evaluate the comfort of four masks: versions of designs A and B customized to his or her face and standardized (Small, Medium, and Large) versions of design A and B. Testing positions involved lying supine, prone, lateral decubitus left and right, and his or her natural sleeping posture. For each position and in each mask the participant was asked to rate his or her comfort on a pre-determined scale.
Data analysis by Tukey’s Multiple Comparison Test (with ɑ = 0.05) indicated that the customized eye shields were not statistically different than wearing no shield at all. The standardized shields were statistically more uncomfortable than wearing no shield at all. Additionally, 70 percent of participants had the least discomfort with one of the customized eye shields. These results suggest that customized eye shields should be pursued commercially over standardized shield design in order to produce the most comfortable experience for consumers.
Team 2: Preventing LVAD Misplacement through 3-D Printing
Manel Djeffal, Alex George, Molly McGown, Alejandro Morales, and Julia Slowey
Advisors: Dr. Yu Chen (Professor, BioE), Nicholas Hiivala (University of Maryland Medical Center)

The left ventricle of the heart is almost entirely responsible for the work in maintaining system circulation; consequently this anatomical feature is the most prone to damage, which can lead to heart failure. Left ventricular assist devices (LVADs) are commonly used as a temporary solution for heart failure patients, but complications may arise due to respective misplacement in the chest cavity. Revolutionary prototyping methods have demonstrated to be a viable method of pre-surgical planning, benefitting both the surgeon and the patient. As such, Team 2’s project proposes a process to prevent misalignment during LVAD implantation and help to standardize the overall process. This process is simply outlined as transforming computed tomography (CT) scans of a patient’s heart and ribs into smoothed 3-D object files. To help visualize the process even further, the LVAD is also developed into a 3-D object file. The files are then 3-D printed for physical interaction by the surgeon such that he or she can find the optimal position of insertion of the LVAD. This process also includes potential to be developed as a standalone software based on the detailed methods. By developing a standard for the LVAD implantation surgery, Team 2 hopes to usher in an age of better recovery for patients with near end stage heart failure.
Team 3: Portable Stroke Rehabilitation System with Real-time EEG Neurofeedback, Sensory Substitution, and Social Engagement
Anastasiya Belyaeva, Elena Galbally, Vasudha Kowtha, Becky Selle, and Jenny Vojtech
Advisors: Dr. George F. Wittenberg (University of Maryland School of Medicine) and Dr. Behtash Babadi (Assistant Professor, Department of Electrical and Computer Engineering and Affiliate Faculty, Institute for Systems Research)
PATENT AWARD

Stroke affects approximately 15 million people worldwide each year. Of these 15 million people, five million are rendered permanently disabled and experience tactile or proprioceptive impairments. Rehabilitation for proprioceptive disabilities is an immensely long and arduous process. Present medical devices improve proprioception through goal-based motion tasks, yet are limited to laboratory space and only provide feedback when the goal is reached. An at-home rehabilitation system is presented that is comprised of a motion-controlled video game, a 3-D motion sensor, a vibrotactile feedback device, an EEG headset, patient analysis software, and a user-friendly online platform. The patient plays a motion-controlled video game that requires them to perform various therapeutic exercises. A device, such as the Kinect One, tracks and records the 3-D location of the patient's upper extremity. The targets in the game are mapped into the reach space of the patient. A vibrotactile wristband is worn by the patient to provide feedback of where the patient is relative to the target. This component utilizes sensory substitution to ultimately improve proprioception. The EEG headset records signals from both hemispheres of the patient's brain to analyze power changes through a multitaper method. Visual neurofeedback trains the patient to subconsciously use their damaged hemisphere and gain greater access to the major motor pathway. Recovery data is analyzed and sent to physical therapists, who can then recommend a new training regime and set thresholds for the patient. Through the platform, patients can participate in multiplayer games and chats or meet-ups. The proposed device is unique to current practice in three key aspects: portability, sociability, and feedback.
Team 4: Accelerated Osteogenesis via Portable Pulsed-Electromagnetic Field Therapeutic Device
Joseph Ecker, TJ Falohun, Guodong Fu, Charles Liu, and Greg Tambini
Advisor: Dr. Yang Tao (Professor, BioE)
The fracture healing process can be very expensive and time-consuming. Additionally, individuals recovering from fractures are often barred from completing basic tasks due to the restrictive size and inflexibility of a cast. Every day that a patient’s recovery time is shortened, valuable time and money is salvaged that can be used productively and allow for them to quickly return to their normal lives.
A fracture is more than just a simple bone break; it is an abrupt interruption in the lifestyle of millions of
Americans each year. In the United States, approximately 6.3 million bone fractures occur annually, with an average recovery time of 8-12 weeks and up to $8000 in direct medical costs. 5-10% of these fractures are categorized as delayed-union or non-union fractures. Such cases are more problematic, often requiring the need for medical intervention due to the inability for the bone to recover on its own due to inadequate blood supply, bone movement, or infection. This condition can result in a recovery time of up to 26 months and up to $45,000 in direct medical expenses.
Pulsed electromagnetic field therapy has emerged as an effective therapy for bone fractures. Studies have shown that the use of electromagnetic fields can cut down the recovery times in fractures by half. Additionally, magnetism circumvents attenuation and safety problems associated with ultrasound; another method of increased healing, and has been approved as a method by the FDA in the past. Over the course of five months, Team 4 designed a portable device that implements PEMF theory in an appealing and effective design that is capable of accelerating bone healing for fracture patients. Team 4’s device – the BoneWelder™ - is unique in design, superior in its effectiveness, and distinctive in its ease of use.
Team 5: Single Incision Cardiac Chest Tube Housing
Nathan Barber, Julie Etheridge, Alex Jankovic, Chavi Rehani, Michael Sikorski
Advisors: Dr. Rawn Salenger (Department of Cardiac Surgery, University of Maryland School of Medicine) and Dr. Christopher Jewell (Assistant Professor, BioE)
SHARK TANK: BEST PROJECT AWARD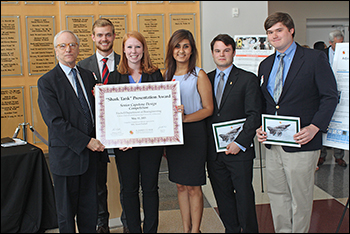
Millions of open-chest surgeries are performed every year. During open-chest surgery, the lungs collapse and the newly-air-filled space between the pleural linings begins to be flooded with fluid. Post-operative bleeding often results in the pooling of blood in the pericardial space. These fluids must be drained in order to avoid complications such as pleural effusion and cardiac tamponade. The current standard of care involves the implementation of a post-operative chest drainage system in which surgeons insert three chest tube catheters before the chest is closed. They then remove the ends, post-operatively, through three separate skin incisions in the upper abdomen.
The need for the three separate incisions results in a bulky, obtrusive network of external tubes that restricts patient movement and prevents patients from becoming mobile more quickly. The drainage tubes can also be quite painful and can severely limit the patient’s ability to participate in any type of physical therapy movements while the tubes are in place. Moreover, the scarring associated with the three incisions for the chest tubes, in addition to the already large incisions necessary for the main open cardiac procedure, is not aesthetically pleasing. Thus, the current standard of care largely disregards patient priorities such as minimizing scarring and physical discomfort.
For six months, Team 5 worked to develop a prototype for a single-incision system in which a housing, inserted into the patient through a single incision and secured in position using sutures, will consolidate the three necessary catheters. Instead of the three tubes exiting the body cavity through separate incisions, they will be able to exit through a single smaller one. The three catheters will be pulled through individual channels in the housing to drain the fluid much as they do now, with the added benefit of increasing patient mobility while reducing the number of incisions, patient pain discomfort, and the amount of unattractive scar tissue as the incision heals. Thanks to an airtight seal, the tubes can continue to be individually managed, as they are now, and removed at separate times without allowing air to enter the chest cavity. The proposed solution also avoids the pitfalls faced by other solutions that require too many alterations to the existing protocol, which discourage clinical adaptation and use.
Team 5’s design is built on an injection molding production model; the team used a 3-D-printed negative mold and a silicone elastomer kit for prototyping. Because this method is inexpensive and allows for rapid prototyping, Team 5’s production model is easily scalable and can yield a product that is both effective and affordable. Team 5 conducted animal and engineering testing. The team’s results show that its housing is easily adapted to clinical use with minimal disruption of existing protocols, and that the use of Team 5’s device does not alter the overall effectiveness of the drainage system (the rate of fluid drainage remains essentially the same).
Open-chest cardiac surgery is no small matter. It often leaves patients with massive bills, in massive pain, with massive scars. Team 5 believes that its simple, affordable device can elevate the standard of care by lessening that pain and discomfort, as well as the souvenir scars.
Team 6: Structural Health Monitoring of Scoliosis Growing Rods
Aminah Asghar, Devon Freudenberger, Brian Goodall, Winston Liu, and Bilal Naved
Advisors: Dr. Adam Hsieh (Associate Professor, BioE, and Associate Chair), Dr. Matthew Oetgen (Orthopaedic Surgery and Sports Medicine, Children’s National Medical Center), and Dr. Byungseok Yoo (Research Associate, Department of Aerospace Engineering)
Team 6’s device will provide a method to monitor the structural health of scoliosis growing rod implants. Scoliosis is the abnormal curvature of the spine and, in severe pediatric cases, the use of growing rods may be used to fix the curvature of a child’s spine. Scoliosis growing rods, however, have been reported to experience high complication rates, including rod fracture, which can lead to unplanned and costly surgery to replace the broken rods. The ability to assess structural health of the growing rods will allow for the intervention and prevention of fractures.
Team 6’s device uses principles of ultrasonic structural health monitoring and guided Lamb waves to assess and detect structural changes in the rods. The system will generate and analyze ultrasonic signals in pediatric growing rods, through biannual ultrasonic probing. Microscale fractures in growth rods presaging failure can be detected through comparison of signal amplitude degradation with older ultrasonic measurements on the rods. The design of the probe adaptors meets the constraints necessitated by the method of sensing and surgery. Future directions of this project include developing a system that integrates individual components into a tableside device for signal processing as well as creating biocompatible, disposable probes to interface with the implant. Team 6’s work demonstrates functional components of such a device for the structural health monitoring of growing rod implants. Further development is required to integrate components into a comprehensive system.
Team 7: Engineering Locally-Sourced Oral Rehydration Solutions
Chris Cherry, Connie Chen, Hannah Hafez, Dan Hogan, and Nariman Ziaee
Advisors: Dr. Ian White (Associate Professor, BioE) and Dr. Chanthap Lon
IMPACT AWARD
Despite the widespread success of modern Oral Rehydration Salts (ORS), over a half-million children in the Developing World continue to die each year from dehydration related to enteric disease. Instead of generating another poorly-adopted externally-conceived solution, this project proposes a new paradigm: partner with communities where ORS has not been affective to develop locally-sourced, culturally-sensitive, and scientifically-tested ORS recipes to be distributed using mobile technology.
Team 8: Adjustable Arm for the Organization and Stabilization of Wires and Tubing
Jordan Hampton, Flannery Loughran, Maeve McCoy, Tara Ruoff, and Talia Sieff
Advisors: Dr. Adam Hsieh (Associate Professor, BioE, and Associate Chair), and Drs. Adnan Bhutta, Jason Custer, and M. Amr Shahnin (Division of Pediatric Critical Care, University of Maryland Medical Center)

When a patient is in the Pediatric Intensive Care Unit (PICU), there are a number of different tubes, wires, and lines to which he or she may be connected. Even more, according to doctors from the University of Maryland Medical Center, one patient may be connected to three to 20 lines at a time for the delivery of medication. After the members of Team 8 paid several visits to the PICU, they realized that the multitude of wires often become tangled, leading to confusion when doctors and nurses deliver medication. Furthermore, the lines and wires make it more difficult to move the patient, because the wires become more disorganized in the process.
Currently, doctors and nurses use their own non-standard ways of keeping track of the wires for proper delivery of medication. Additionally, nurses spend valuable time disentangling the wires, as it is necessary. While there are a few products on the market that target the stabilization of the endotracheal tube, Team 8’s patent research indicated that there is an unmet need for a device to organize wires attached to the patient – particularly the small patients in the PICU.
With this in mind, Team 8’s goal is to introduce a device intended to organize lines and wires to make it easier for nurses and doctors to deliver medication and move the patient without tangling the wires. The result of the engineering design process is Team 8’s final product, an Adjustable Arm for the Organization and Stabilization of Wires and Tubing. The arm is equipped with a clamp so that it can be fastened to the IV stand, which is always moved in conjunction with the patient, and has a telescoping feature which allows its position to change relative to the patient. Most importantly, the end nearest the patient is fitted with a plate with ports for up to 21 wires. The device is designed so that it will not come into contact with the patient and will not cover the patient’s chest, so as to not interfere with chest X-rays and doctors’ access to the patient.
Team 9: 3-D Printed Patient-Specific Pulmonary Models as a Preoperative Method
Brittany Greene, Priyanka Jayanti, Fatemeh Khouzaei, Kelly Leimkuhler, Ashley Matos, Zurana Taluckder
Advisors: Dr. John Fisher (Fischell Family Distinguished Professor and Associate Chair, BioE) and Dr. Ashutosh Sachdeva (University of Maryland Medical Center)
STUDENTS' CHOICE

Doctors have been using non-specific models of the human body for years. Unfortunately, the models the doctors use are usually very general and are not applicable in all situations – such as when using cadavers. As such, Team 9 proposed a process by which doctors will be able to use patient specific CT scans of the chest cavity to create 3-D printed models of the pulmonary pathways on which they will be performing medical procedures. The advantage of these patient-specific models would be that they reflect exactly what the doctor will be working on inside a patient’s body. It will reduce surgery time and the amount of anesthesia given to a patient, and make the entire procedure more efficient. Within the process, the CT scans will be converted into 3-D computer models using Mimics and 3-Matic, and will then be printed. The models themselves will be made of a rubberlike material that will mimic the properties of an actual pulmonary pathway to serve as an enhanced preoperative method that will enhance surgical planning.
Team 10: SensiMatt: A Dynamic Pressure Relieving Medical Mattress
Zack Brandes, Meghan O’Lone, Nitish Malladi, Grace Wang, and Andrew Wesley
Advisors: Dr. Jeffrey Hasday (Pulmonary and Critical Care Medicine, University of Maryland School of Medicine) and Dr. Yang Tao (Professor, BioE)
SECOND PLACE
One to 3 million people develop bedsores each year in the United States alone, and treatment for these bedsores costs up to $11 billion. Bedridden hospital patients and nursing home residents often develop bedsores from the continuous pressure of a mattress pushing against soft tissue, restricting blood flow, and subsequently killing the tissue. Not only are bedsores extremely painful and uncomfortable, but they also pose a very serious risk to life and overall health. To prevent the development of bedsores and allow for the proper healing of bedsores and other wounds, sensitive areas should never be subjected to the high pressure normally experienced by lying on a bed.
Existing products designed to combat bedsores involve alternating high and low pressure throughout the mattress so no single area is subjected to high pressure all of the time. Subjecting sensitive areas to high pressure for even a short time, however, is unacceptable. To solve this problem, Team 10 developed a multi-cellular air mattress, SensiMatt, that can automatically localize a wound or developing bedsore and modulate the air cell inflation pattern to constantly maintain low pressure on this target area.
SensiMatt presents a unique and viable solution to this problem that differs from current approaches in two ways. First, SensiMatt can create an area of low pressure anywhere on the bed, while still maintaining high pressure everywhere else. Second, SensiMatt can dynamically localize the wound or bedsore, even as the patient changes position. Team 10 has constructed a working prototype at a 1:2 scale model size of a standard medical mattress. With proper funding, the team hopes to fabricate a full-sized model that is hospital- and nursing home-ready and will help the sick and elderly maintain a higher quality of life.
Team 11: Pitch Perfect-ed: Real-Time Monitoring of Arm Motion to Prevent Injury
Brendan Booth, Kelly Camp, Menenu Duson, Matthew Kelleher, and Corey Roller
Advisors: Dr. Hubert Montas (Associate Professor, BioE) and Dr. Michael April (Greater Washington Pain Management)

Ulnar collateral ligament (UCL) damage is a real fear for competitive baseball players. The repetitive stress caused in the elbow from the motion of throwing a baseball can cause small or large tears in the UCL. Common symptoms of UCL damage are pain in the elbow, instability in the elbow, and a decreased ability to throw overhead. The last symptom can be devastating for serious ballplayers. Currently, the most common procedure to fix a torn UCL is known as Tommy John surgery. Recovery from this procedure takes a minimum nine months, but often it takes professional pitchers a full year to return to the competitive scene.
While current treatments are designed to help an already injured UCL heal, the Pitch Perfect-ed design aims to proactively prevent UCL injuries from occurring. The sleeve uses accelerometers and gyroscopes to measure the velocity and forces inside the elbow joint during a throwing motion to determine if the user is under a risk of ligament damage. The sleeve then communicates with the user through a smartphone application via Bluetooth technology.
The data gathered from the sensors during a throw are processed through unique algorithms in order to display forces and velocities experienced by the UCL. The sleeve contains two combination accelerometer/gyroscope sensors placed on the dorsal side of the upper arm and forearm at a set distance from the elbow joint, where the TinyDuino and Bluetooth are located. The accelerometer measures dynamic acceleration and can analyze the way the elbow moves during the throw. The gyroscope is used to detect orientation and rotation of the elbow. The combination of the two types of sensors provides a vast amount of accurate information about what really happens inside a throwers elbow. In addition to the sleeve, a smartphone application has been created to connect the users of the product to the information gathered by the sleeve. All the sensors are connected to the application via Bluetooth. The application allows the user to input individual body metrics that contribute to personalized force calculations which are presented following each throw. The Pitch Perfect-ed system combines innovative wearable technology, Bluetooth communication, and a user-friendly smartphone application to prevent UCL injury.
Team 12: Lift-Safe: Preventing Lower-Back Pain in the Workplace
Sean Connolly, Anthony Dinh, Corey Koller, Christopher Meyer, and Gaurav Nayyar
Advisors: Dr. Michael April (Greater Washington Pain Management), Dr. Marc Cohen (Weill Cornell Physicians), Dr. Martha Connolly (Director, Maryland Industrial Partnerships, Mtech), Dr. Adam Hsieh (Associate Professor and Associate Chair, BioE), (Ben Woodward (Biotechnology Research and Education Program, Mtech), Dr. Yang Tao (Professor, BioE)
BEST IN LEAN LAUNCHPAD BUSINESS MODEL
Incidents relating to lower back pain are estimated to incur economic costs of approximately $194 billion per year. This is of particular interest to maintenance companies, such as FedEx and Walmart, who want to maximize ergonomics for each employee, while minimizing costs. Although devices such as lifting belts are intended to help prevent injuries to those in manual materials handling occupations, they are not equipped to monitor usage.
Team 12 developed an algorithm to track and detect improper lifting movements to address the issue of lower back pain. This algorithm has the potential to offer clients significant savings by decreasing the dollar amount spent on workmen’s compensation by at least 20 percent, yielding a potential $40 billion in total savings. The system that Team 12 developed uses a modified version of an existing device, the YEI 3-Space Sensor, which is attached at the lower back using a belt clip. It has the ability to track each of the movements the employee performs throughout the day. At the end of the day/week, the data collected will be run through the algorithm to detect whether these movements are proper or improper. Using this system, we have demonstrated feasibility and were able to detect what proper and improper movements should look like. Currently, Team 12 is focusing on improving the algorithm by taking into account more variables, such as walking and running, and nulling out that data. Team 12 has steadily made progress and will be releasing an updated algorithm that can detect more incorrect movements within the next six months.
Team 13: NAP’D: Neonatal Acoustic Protection Device
Louis Born, Erin Kreeger, Makenzie Miller, Siddarth Plakkot, Alyssa Sims
Advisors: Dr. Rose M. Viscardi (University of Maryland School of Medicine), Dr. Yang Tao (Professor, BioE)
FIRST PLACE
Sensorineural hearing loss is a major risk for infants who remain in the neonatal intensive care unit (NICU) for extended periods of time. Noise produced by life supporting machines and other sources results in sound levels reaching as high as 90 decibels (dB) on a daily basis. As a result, 52 percent of preterm infants who were cared for in incubators are reported to leave the NICU with abnormal audiograms.
Current methods of protecting infant hearing do not reduce noise to the 45 decibel level recommended by the American Academy of Pediatrics. Knowing this, Team 13 proposes a device that integrates noise-cancelling technology into a comfortable cap that infants can wear on a daily basis to protect their hearing. The team fabricated ear cups containing speakers out of flexible material and arranged all the components on an elastic, adjustable band that can be easily inserted into a knit cap of any size. Their device provides both passive and active noise cancellation through its design and electrical components, as well as the capability for beneficial audio integration using Bluetooth technology.
Team 14: Mobile iCP: A Non-invasive Intracranial Pressure Monitor
Nayeem Chowdhury, Carolyn Kleinberger, Hannah Ornstein, Michelle Patkin, Rebecca Stevick
Advisors: Dr. Hubert Montas (Associate Professor, BioE), Dr. Gunjan Parikh (University of Maryland School of Medicine)
SHARK TANK: MOST CREATIVE PROJECT AWARD
Traumatic brain injury (TBI) accounts for 30 percent of all injuryrelated deaths in the U.S.
One way to measure the severity of TBI is to examine the rise in intracranial pressure (ICP), as it occurs due to swelling in the brain. The optic nerve sheath (ONS) dilates when the ICP increases, and this correlation has been clinically calculated. Unfortunately, current ICP detection methods are invasive, expensive, subject the patient to high levels of radiation, and require medical professionals.
Recognizing this, Team 14 has developed the Mobile iCP system: a portable, user-friendly device that enables self-monitoring of ICP. The device uses a sonogram of the eye to produce an image of the ONS, and a mobile application to measure the diameter of the ONS. The Windows phone application then calculates the ICP based on the ONS diameter, and produces a clinical diagnosis. Since the device automatically computes the ONS, it decreases the potential for error and eliminates the need for a medical professional, Team 14 says.
The team also developed an automated headgear system to allow for long-term, handsfree monitoring of ICP. Using the headgear device, a remote doctor would be able to monitor the ONS diameter. The Mobile iCP system could be useful in a civilian firstresponse application or military setting to help monitor the severity of TBI and allow for better evaluation and triage. Additionally, patients with slow-growing brain tumors or those at high risk of stroke can benefit greatly from this style of monitoring, according to Team 14.
The application and detection methods were validated using a fabricated eyeball model. This spherical model made from psyllium powder and gelatin mimics the attenuation in a physiological eye. The team found that the code was accurate within 6.1 percent of the known diameters of the model optic nerves.
Further testing to confirm the team’s mobile application results is underway in the neuro ICU of the University of Maryland Medical Center in Baltimore. As a whole, the Mobile iCP system provides an accurate, noninvasive, and user-friendly method for measuring increased ICP due to TBI.
Team 15: Low-Cost Ankle Rehabilitation Robot for Children with Cerebral Palsy
Wenqi Han, Byeol Kim, Pierce Radecki, Peyi Runsewe, and Robert Vinson
Advisors: Dr. Kevin Cleary (Sheikh Zayed Institute for Pediatric Surgical Innovation, Children’s National Health System), Dr. Jae Kun Shim (Associate Professor, Department of Kinesiology)

Robotic rehabilitation is a promising new field with applications in physical therapy, bioengineering, and kinesiology research. Through the use of robotics, the rehabilitation process can see several benefits, including the ability to quantify and optimize therapy.
In this project, Team 15 presents a low-cost robotic rehabilitation system targeting the needs of children with cerebral palsy who are currently undergoing ankle therapy. The team’s device specifically addresses the shortcomings of previous efforts by the following: it utilizes a simple mechanical system, is capable of replicating sophisticated ankle motions, and is designed to simplify the manufacturing process to reduce costs to the consumer. The device consists of a footplate attached to an array of three linear feedback actuators, each controlled by a respective control board, which are coordinated together via a laptop computer. Additionally, the device is lightweight, compact, and affordable for most patients, allowing the device to be personally owned or leased for at-home use.
Subsequently, Team 15 believes children with cerebral palsy will have a convenient means by which to achieve reproducible physical therapy in the comfort of their own homes, saving valuable time for both the children and their families who would otherwise be forced to commute to a physical therapist’s office. Future plans for the device include the development of a video game interface, addition of a translational degree of freedom, passive resistance capabilities, and expansion of the consumer base to athletic rehabilitation and strength training.
Team 16: Clinical Sleeve for ACL Injury Risk Assessment
Alex Chase, John Mann, Eugene Perelshteyn, Alec Simon, and Justin Wisor
Advisors: Dr. Michael April (Pain and Injury Center of Greater Washington), Mr. Marc Cohen (Assistant Research Scientist, University of Maryland Institute for Systems Research), Dr. Adam Hsieh (Associate Professor, BioE, and Associate Chair)
Anterior cruciate ligament injury is a serious and sometimes preventable problem that many athletes face. A previously injured ACL has a 15 times greater chance of injury within the 12 months immediately following the first injury. Proper exercise and response to improper form when an athlete is using their ACL can help to lower the number of ACL injury incidences, so identification of improper use of a person’s ACL can help prevent injury.
Team 16 sought an opportunity to design a clinical knee sleeve for ACL injury risk assessment. Their carefully designed sleeve is embedded with an accelerometer which feeds data to an external microcontroller using I^2C communication. The accelerometer is tasked with giving data about the accelerations in three directions, and it offers the comparison of the three different readings to allow for proper interpretation. This data can then be recorded by CoolTerm and processed by Matlab, which takes the collected data and creates a graphical representation.
The team’s goal is to provide physicians with the opportunity to analyze the graphical data and make a quantifiable decision about the risk that the patient has for tearing their ACL. The team’s vision is that, in response to data collected, a physician would be able to assign the patient different collections of exercises that can strengthen the muscles and decrease the patient’s risk for tearing his or her ACL.
Team 17: Intelligent Collector: Efficient Tool to Sample Pleural Fluid
Lampouguin Y. Douti, Jean-Paul Littleton, Max Arifin, Kenneth Wesley Bryant, and Whitney Wilson
Advisors: Dr. Keith Herold (Associate Professor, BioE), Dr. Robert M. Reed (Pulmonary and Critical Care, University of Maryland Medical Center)
Pleural effusion is an abnormal excess accumulation of fluid in the pleural cavity of the lungs, resulting from factors such as pneumonia, cancer, or post-surgery complications. The current system for pleural effusion collection consists mostly of health professionals working to take fluid samples by inserting a syringe into a collection chest tube. This method of extraction is not efficient because patients do not always maintain consistent levels of fluid. Even more, pulmonary doctors face the unique challenge of quantifying the concentration of the different particles, protein and albumin present in the collected fluid. This lack of an efficient sampling method can result in a doctor's decreased access to important information that could influence the patient’s diagnosis and course of treatment.
Given this, Team 17 proposed a device that offers a pleural effusion sampling system that allows for smooth collection of pleural liquid from the patient. It functions as a small reservoir that collects 30-60mL of fluid and provide easy access and manipulation to the user, nurse. The collection reservoir is a removable cylindrical tube enclosed in a 7 inches tall box. The drainage tube connects to either side of the device, allowing it to be easily integrated into the current drainage system. In addition, the device is able to calculate the flow rate of the pleural effusion leaving the patient as well as alert the nurse when the sample is ready to be collected via an LED indicator. These additional features accomplish the task of making the job of sampling effusion fluid easier, provide doctors with fluid flow rate information, useful to shed light on preliminary diagnosis on patient’s current health status, and supplement doctors with enough fluid for further lab testing.
Team 18: A Novel Coupling Gel System for Ultrasound-Guided Injections
Adeola Awowale, Kyle Kenney, Chelsea Kraynak, Stephanie Okorafor, and Trina Quabili
Advisors: Dr. Paul Bigeleisen (University of Maryland Medical Center), Dr. John Fisher (Fischell Family Distinguished Professor and Associate Chair, BioE)

With increasing portability of ultrasounds, ultrasound guided injections have become widespread in recent years. Orthopedic surgeons, anesthesiologists, and physical therapists commonly use ultrasound-guided injections to administer cortisone shots, joint lubricants, and local anesthetics. Case studies have reported that the placement of needles using ultrasounds is 97 percent accurate; however, once the needle is correctly positioned, maintaining the correct position becomes problematic. Therefore, establishing an improved method of maintaining precision during ultrasound-guided injections is necessary.
Team 18’s capstone project is aimed at developing a new viscous coupling agent between the ultrasound probe and the skin to replace traditional propylene glycol. The goal of this modification is to increase probe stability after identifying a specific subcutaneous structure, so that an ultrasound-guided injection can be administered easily. This new coupling agent is required to be both gelatinous and slippery at the beginning of the scan, with attenuation similar to tissue so that ultrasound data can be obtained through the material.
The team has worked with a new, cutting-edge ultrasound gel that increases viscosity with increasing temperature, within 30 to 60 seconds. Additionally, the team uses a probe attachment developed to maximize the surface area between the probe, skin, and coupling gel. This will allow the doctor to more easily administer precise injections. The team’s ultimate goal is that this new viscous coupling agent and probe attachment becomes the standard interface for modern ultrasound procedures requiring injection, to replace standard propylene glycol when probe security is needed.
Congratulations!
The Fischell Department of Bioengineering would like to congratulate all who participated in this year's Senior Capstone Design Competition and wish the Class of 2015 the best of luck in all future endeavors.
Thank you!
The 2015 BioE seniors would like to thank their professors and mentors (listed with their Capstone teams above); lab staff including Melvin Hill for guidance, time, and labor; administrative staff members for help with financial support and purchasing; Professors Yang Tao and William E. Bentley; the 2015 judges; and friends in outside academia and industry for the advice and supplies they donated that helped these projects succeed.
View the full 2015 Capstone Design Competition photo gallery.
Published May 28, 2015