News Story
Spine Society Grant Supports Hsieh's Back Pain Research

BioE Associate Professor Adam Hsieh (right) with fellow NASS grant recipients.
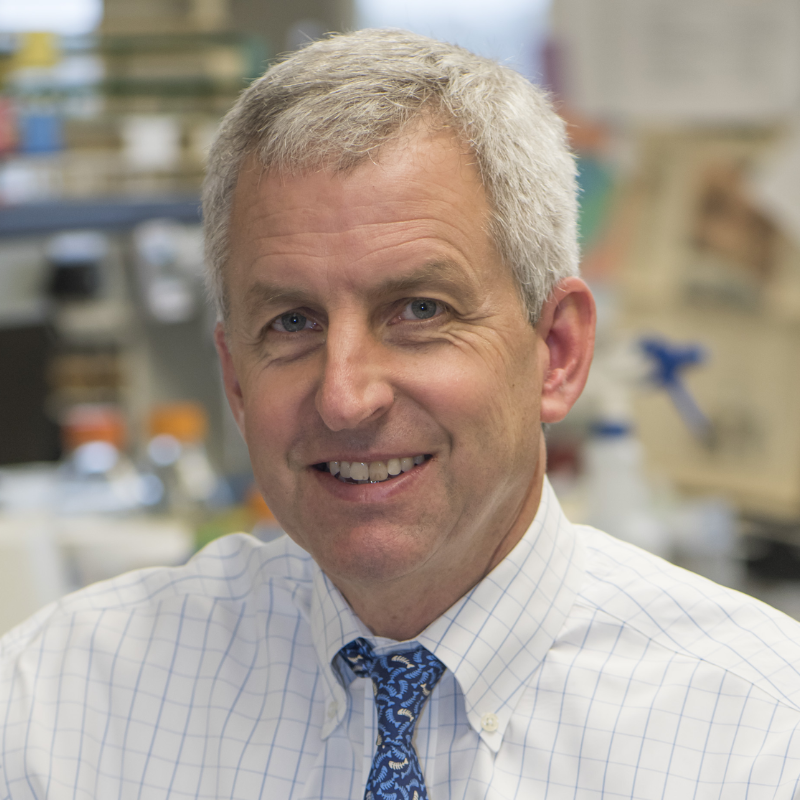
Clark School Fischell Department of Bioengineering (BioE) Associate Professor Adam Hsieh has received a Basic Research Grant from the North American Spine Society (NASS) to explore and explain the exact biological mechanisms that lead to back pain.
"While there have been significant advances in identifying the risk factors of spinal disorders associated with lower back pain, they don't address the problem faced by those who are already afflicted," Hsieh explains. "Although recent studies have made progress toward understanding what factors might provoke chronic intervertebral disc pain, the precise biological mechanisms responsible for it remain poorly understood."
He describes the project, in which he will partner with co-PI and former BioE professor Sameer Shah (University of California, San Diego), as an early step in a broader effort to improve the diagnosis and treatment of discogenic back pain through a more comprehensive understanding of what happens at the cellular and molecular levels.
Hsieh and his colleagues have recently developed a novel in vitro culture model of the spine's dorsal (back) root ganglions, the small bulb-like nodules to which nerve filaments extending from the spinal cord connect. The model allows them to study the cellular physiology and regulation behind the invasion of nerves called sensory axons into the extracellular matrix, the fluid found between the cartilage cells in intervertebral discs. When the nerves penetrate, the discs become sensitized to the mechanical pressures of their environment, resulting in pain.
Hsieh and Shah will explore how inflammatory conditions in the spine affect the communication between the dorsal root ganglions and the intervertebral disc's annulus fibrosis, the stiff ring of fibrous material around its gel-like center. It is this intercellular communication that is thought to stimulate the pain-inducing neural growth. Understanding how to control or block this chatter could stop it; however, Hsieh says, things aren't so straightforward, and are sometimes even contradictory.
"Not all discs invaded by nerves are painful, and some painful discs don't exhibit pronounced nerve penetration," he says. "This represents a critical gap in our knowledge, and suggests that the regulation of both neuronal growth and sensitization processes are complex. Inflammation inhibits neural growth, but stimulates disc cells to secrete nerve growth factor. The degradation of the extracellular matrix removes barriers to nerve ingrowth, but decreased tissue stiffness blocks it. Mechanical and nutritional considerations present additional complexities. Our hypothesis is that a confluence of biochemical and biophysical factors result in neuronal ingrowth, neurophysiological sensitization, and pain. While individual connections have been made between inflammation, disc cells, neurons, and extracellular matrix degradation, the complete picture has yet to be uncovered."
Published November 20, 2013