News Story
UMD Researchers Point to Future of Engineered Immune Tissues

Illustration: Jennifer Fairman
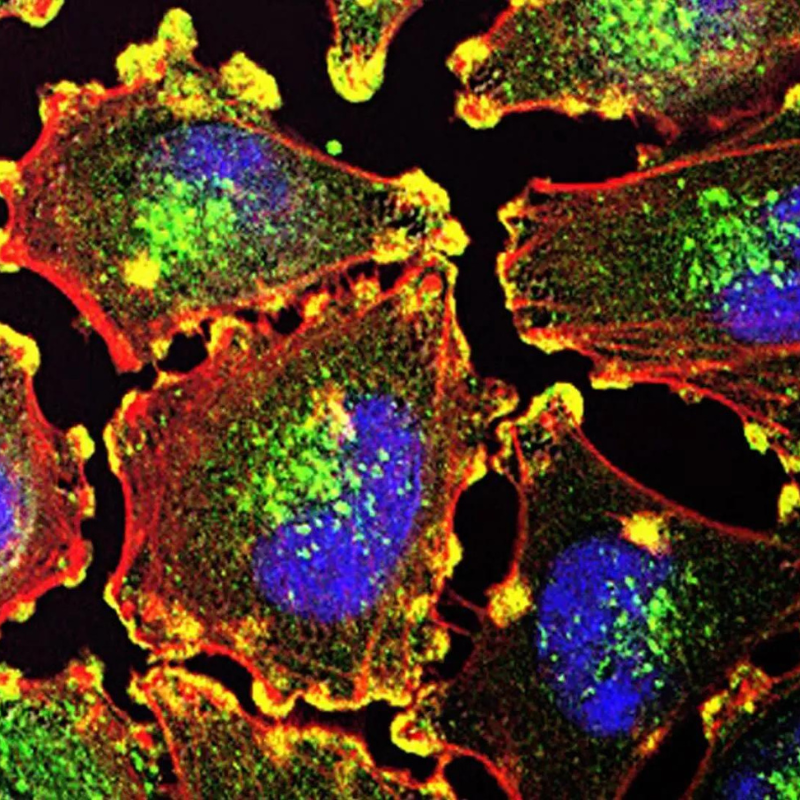
Researchers at the University of Maryland, College Park and Baltimore campuses are working to shed new light on how, one day, immune tissues could be designed and implanted to create next-generation vaccines or immunotherapies for a range of diseases, or serve as cutting-edge tools for the early diagnosis of cancers or other illnesses.
The group’s review was published this week as the cover story in the June print edition of Nature Materials.
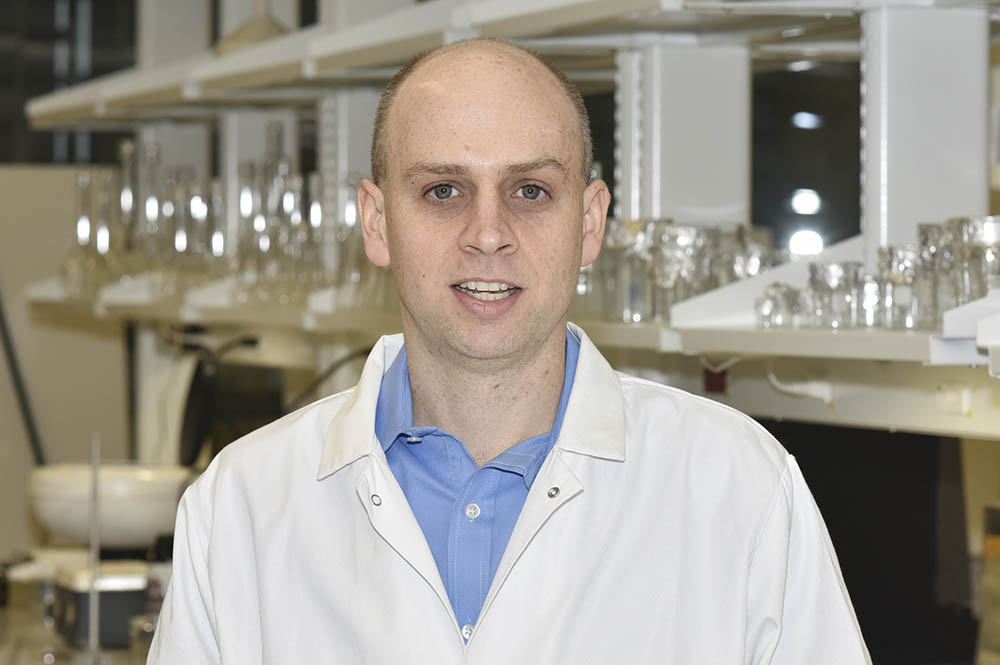
“One day engineers might be able to design immune tissues for implantation into patients to generate the exact immune responses needed to fight a disease such as cancer without side effects,” said University of Maryland (UMD) Fischell Department of Bioengineering (BIOE) Associate Professor Christopher Jewell, corresponding author on the paper, principal investigator of the BIOE Immune Engineering Lab, and a Robert E. Fischell Institute for Biomedical Devices faculty member. “These technologies might also create accurate immune tissue models that enable rapid screening of vaccines or immunotherapies outside the body.”
Today, vaccines and immunotherapies provide benefits for human health ranging from the eradication of diseases to improved outcomes for patients with cancer or autoimmune disease. But, there exists a fundamental disconnect between where vaccines and immunotherapies are studied – in cell culture and animal models – and their application to humans.
Recognizing this, researchers in the immunoengineering field are hopeful that engineered immune tissues and organs – such as bone marrow, lymph nodes, and spleen – could be used as in vitro tools to more accurately study human immune function and diagnose disease. Ultimately, immune tissues engineered for implantation could serve as vaccines or immunotherapies capable of on-demand control to produce immune responses tailored for specific infections or disease.
“The field of bioengineering has advanced to the point that we understand at least some of the ways in which chemistry and material properties – such as mechanical stiffness and 3D structure – impact immunological function and regulation,” Jewell said. “The field is starting to put these two areas together to recreate very complicated immune functions, but much of the work thus far has been in controlled settings. As such, these advances could provide new opportunities anywhere in which the immune system is involved in either fighting or causing disease. This covers infection, cancer, autoimmunity, transplantation, and many other areas where great unmet medical needs exist.”
“There are major important and imaginative advances highlighted by this review,” said Jonathan Bromberg, Professor of Surgery and Microbiology and Immunology at the University of Maryland School of Medicine, and a co-author of the Nature Materials paper. “First is the combination of immunologic and materials sciences approaches to guide and control the immune response. Second, is the possibility of creating not only ‘positive’ vaccines that generate proinflammatory or curative immune responses for cancer or infectious diseases, but also ‘negative’ vaccines that prevent or curtail responses for autoimmunity or transplantation.”
Current clinical translation of vaccines and immunotherapies is generally inefficient as it relies on trial-and-error methods and testing in cells and animals, then in humans.
Even more, this approach does not provide a complete picture of how vaccines and immunotherapies will ultimately perform in humans, Jewell said. As such, engineered immune tissues could also serve as important tools for studying immune function outside the body.
“Researchers do a lot of work in cell cultures and animal models, but both have limitations,” Jewell said. “In the case of cell cultures, most often, researchers work with 2D cultures; but, everything in the body is three-dimensional. And, if you’re working with one or a few cell types in culture, the results could be very different from what they might be in the human body where there is a heterogeneous mixture of cells everywhere. This is significant because the types of immune responses that develop during disease are impacted by all of these characteristics.”
Fortunately, immunology researchers – like those in Jewell’s lab and at the University of Maryland School of Medicine – are making progress. Last year, Jewell’s group demonstrated that, by controlling the local signaling environment in a lymph node, the specificity and effectiveness of an immune response throughout the entire body can be controlled without systemic exposure. Their findings were published in Cell Reports.
“The knowledge base in immunology, materials science and engineering is sophisticated enough – and there are enough researchers working at the interface with sufficient momentum and cooperativity – that we’re able to see that breakthroughs are possible,” Jewell said.”
BIOE graduate students Emily Gosselin and Haleigh Eppler served as lead author and contributing author for the Nature Materials article, respectively.
Published May 23, 2018